Global competition in health care is allowing more patients from developed countries to travel for medical reasons to regions once characterized as “third world.” Many of these “medical tourists” are not wealthy, but are seeking high quality medical care at affordable prices. To meet the growing demand, entrepreneurs are building technologically advanced facilities in India, Thailand, Latin America and elsewhere, and are hiring physicians, technicians and nurses trained to American and European standards to run them.
How Patients Obtain Treatment Abroad. Patients usually coordinate their treatment through medical travel intermediaries. These services often employ doctors and nurses to assess the medical efficacy of procedures and help select physicians and hospitals. Some services are affiliated with specific medical providers and send patients exclusively to those hospitals. Currently, the treatment networks of most U.S. health insurers do not include foreign providers. But since six million people a year worldwide are expected to travel for medical care by 2010, that is quickly changing.
More Health Plans Cover Medical Travel. BlueShield of California has a health plan, Access Baja, designed for Americans and Mexicans who choose to receive medical care in northern Mexico. In 2007, BlueCross BlueShield of South Carolina established Companion Global Healthcare, a network of foreign-based hospitals that includes internationally accredited medical facilities in Singapore, Thailand, Turkey, Costa Rica and Ireland.
Denver-based BridgeHealth International also has a provider network of offshore hospitals, clinics and physicians. It works with insurers and employer health plans to facilitate workers' treatment abroad. Insurers Aetna and Cigna both report growing interest in medical tourism among employers. Mercer Health, an employee benefits consulting firm, is helping several Fortune 500 employers use medical travel to help stem the rising cost of employer-provided medical coverage.
Indeed, a report by the International Foundation of Employee Benefit Plans found that 11 percent of employer health plans surveyed now cover medical travel.
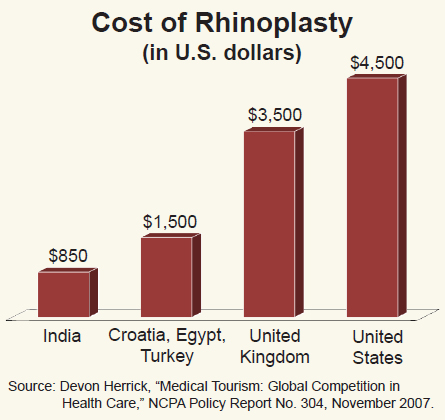
Treatment Abroad Costs Less. Fees for treatments abroad range from one-half to as little as one-fifth the price in the United States, depending upon the destination country and type of procedure performed. For example:
- Apollo Hospital in New Delhi, India, charges $4,000 for cardiac surgery, compared to about $30,000 in the United States.
- A rhinoplasty (nose reconstruction) procedure that costs only $850 in India would cost $4,500 in the United States. [See the figure.]
- An MRI in Brazil, Costa Rica, India, Mexico, Singapore or Thailand costs from $200 to $300, compared to more than $1,000 in the United States.
 Why Treatment Abroad Costs Less. There are many reasons why medical costs are lower abroad.
Why Treatment Abroad Costs Less. There are many reasons why medical costs are lower abroad.
Lower Labor Costs. In the United States, labor costs equal more than half of hospital operating revenue, on the average. Yet, Indian physicians often earn only 40 percent as much, and many Indian nurses earn only one-tenth as much, as their American counterparts.
Less Third-Party Payment. In the United States, patients spend only 13 cents out of pocket for every dollar they spend on health care; insurers or government pay the rest. In countries with growing, entrepreneurial medical markets patients pay more out of pocket. For instance, local patients payout of pocket for 51 percent of health care in Mexico and 78 percent in India. Consequently, providers must compete for patients based on price.
Limited Malpractice Liability. Malpractice litigation costs are lower outside the United States. American physicians in some specialties pay more than $100,000 annually for liability insurance, while a physician in Thailand spends about $5,000 per year.
Price Discrimination. Medical suppliers often charge customers in lower income countries less than customers in higher income countries for the same product or service. As a result, hospitals in developing countries pay much lower prices for medical supplies, equipment and drugs than do hospitals in rich countries. For instance, wholesale prices for the artificial joints and other equipment used in hip replacements are much less in India than in the United States.
Measuring Quality. Many health care providers in developing countries meet U.S. health quality standards. In fact, more than 120 hospitals abroad are accredited by the Joint Commission International (JCI), an arm of the organization that accredits American hospitals participating in Medicare. Moreover, many foreign hospitals hire physicians who are U.S. board-certified, or have internationally respected credentials. And many of the physicians were trained in the United States, Australia, Canada or Europe.
Obstacles to Medical Tourism. Outdated laws and regulations create barriers to medical tourism. For example, the federal Employee Retirement Income Security Act (ERISA) could make it difficult for U.S. providers to offer financial rewards to willing medical tourists without being exposed to increased liability risk. State laws that require doctors to be licensed in the state where the patient receives treatment are another problem. Such laws prevent medical tasks from being performed by providers in other states or countries.
What Public Policy Changes Are Needed? The first step for state and federal policymakers is to understand that global competition in health care will benefit American consumers by reducing costs and improving quality through competition. But other action is also needed.
Modernize State Licensing Laws. Medical licensing laws should be brought into the information age, where distance (or country) is irrelevant in procuring many medical services. Foreign physicians who meet standard criteria should be considered licensed if their skills have been evaluated and approved for inclusion in an insurer's network.
Allow Financial Incentives. Insurers and employer-sponsored health plans should be able to offer financial incentives for seeking care abroad, much as they do currently for medical services within their network, without facing increased liability risks. Legislation such as ERISA should not penalize providers who offer lower cost treatment options for patients willing to travel overseas for care.
Lead by Example. Federal and state government should lead by example, by allowing Medicare and Medicaid programs to send willing patients abroad. Medicare would particularly benefit from cost savings since it pays for a large volume of orthopedic and cardiac procedures.
Conclusion. As more insured patients begin to travel abroad for low-cost medical procedures, medical tourism will result in sorely needed competition in the American health care industry.
Devon Herrick is a senior fellow at the National Center for Policy Analysis.