Health care spending per person varies widely across the country, but greater spending does not appear to produce better quality. A natural inference is that some areas of the country are less efficient in the use of health care resources.
Thus, it is argued that health spending could be cut substantially if the high-spending areas practiced medicine in the same way as the low-spending areas. Office of Management and Budget Director Peter Orszag, for example, argues that health care spending for the country as a whole could be reduced by $700 billion a year. But how can these savings be realized?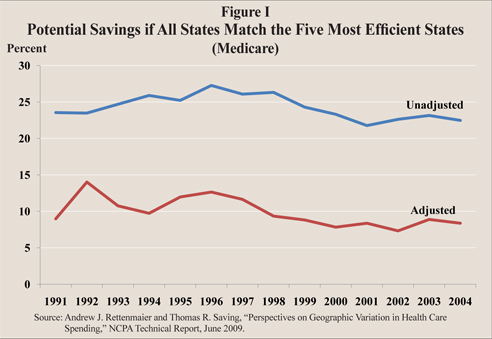
Medicare Spending Variation. A number of studies have found that Medicare spending varies substantially from one state, county or hospital region to another. For example:
- In 2004, average Medicare spending in Louisiana (the highest spending state) was $8,659 while spending in South Dakota (the lowest spending state) was $5,640, almost 35 percent less.
- Taken as a group, Louisiana, Maryland, New Jersey, Florida and Texas averaged more than $8,200 in 2004, or about $800 above the national average for Medicare spending.
- By contrast, South Dakota, Montana, New Mexico, Hawaii and Idaho all spent less than $5,800 – about 40 percent less than the states at the top of the distribution.
- Overall, if every state were as "efficient" as the fifth lowest spending state, Medicare spend-ing could be reduced by about 25 percent.
These numbers appear to confirm Orszag's claim without answering the question of how we could dramatically change the practice of medicine in 45 states. However, before concluding that there are large potential savings, there are two important factors that need to be considered.
Spending on Other Patient Groups by State. News stories often imply that doctors in high-spending Medicare states are practicing medicine in a way different from doctors in low-spending states. One is left to infer that this must also be true for Medicaid patients and private patients as well. But this inference is not entirely true.
For example, although Louisiana is the highest spending Medicare state and South Dakota is the lowest, average per capita health care spending for the whole population is actually lower in Louisiana ($5,040) than it is in South Dakota ($5,327). This is not an isolated case:
- Although Texas is fifth highest in Medicare spending per capita, it is 43rd in per capita spending for the state's entire population.
- California is 11th in Medicare spending, but 42nd overall.
- North Dakota is 43rd for Medicare, but 11th overall.
It appears that high Medicare spending is often associated with lower spending on the non-Medicare/Medicaid population and vice-versa. This observation is consistent with cost shifting between public and private payers, although there may be other explanations as well.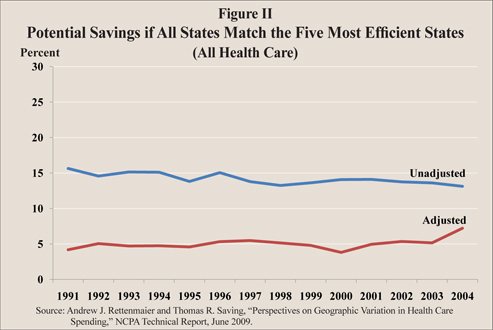
Adjusting for State Characteristics. Differences in state characteristics, including demographics, income, health status and the peculiarities of state health care markets, must also be considered. For example:
- Spending typically is higher the poorer the population's health, the older their age and the higher their income.
- Higher income maintenance payments are also associated with higher Medicare spending and population-wide spending.
- Higher uninsured rates are associated with higher Medicare spending but, as expected, lower health care spending by the non-Medicare/Medicaid population.
So in order to estimate potential savings, we must adjust for these factors. [See Figure I.]
Measuring Potential Savings. After adjusting for differences in state characteristics, we can re-examine the original premise. Suppose that we could induce doctors everywhere to practice medicine the same way it is practiced in the fifth lowest spending state. Based on the experience over a 14-year period, the potential savings across all populations is only about 5 percent! [See Figure II.]
Of course, changing the practice of medicine in 45 states would entail administrative costs. Patients could potentially be harmed in the process. As practical matter there are probably no savings to be had at all.
Implications for a "Public Plan." A health reform proposed by President Obama and being considered by Congress would erect a system parallel to our employer-based private health insurance system, called an "exchange." Within the exchange, people would have choices of health plans, and a highly contentious issue is whether one of the choices should be a public plan (for example, Medicare for nonseniors and the nondisabled).
Our results show that the greatest persistence in this spending variation over time is in Medicare and that the potential savings are greatest in the Medicare sector. Spending variation in the private (non-Medicare/Medicaid) sector is less persistent. This suggests that an expansion of a Medicare-type program could make the problem of "waste" worse, not better.
Andrew J. Rettenmaier and Thomas R. Saving are executive associate director and director, respectively, of the Private Enterprise Research Center at Texas A&M University and senior fellows with the National Center for Policy Analysis.
* See Andrew J. Rettenmaier and Thomas R. Saving, "Perspectives on Geographic Variation in Health Care Spending," NCPA Technical Report, June 2009, for a discussion of the data and findings reported here.