Under the new health care law, most U.S. residents will be required to have health insurance by 2014. About 32 million additional people are expected to enroll in some type of health plan. Evidence suggests that insured people consume twice as much medical care as uninsured people, other things being equal. This means that 32 million people will try to double their consumption of medical care. Yet, who will provide that care?
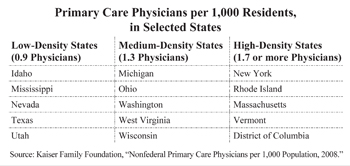 According to the Journal of the American Medical Association, there are 778,000 practicing doctors in the United States. Just under half of them are primary care physicians. Even before health reform, the Association of American Medical Colleges estimated that an additional 45,000 primary care physicians would be needed by 2020 to keep up with demand. Already, the availability of primary care physicians varies significantly by region and among states: from 0.9 to 1.0 per 1,000 population in many Southern and Western states to between 1.4 and 2.8 per 1,000 in the Northeast. This means there are about twice as many doctors per 1,000 residents in the Northeast than in states such as Texas. [See the table.]
According to the Journal of the American Medical Association, there are 778,000 practicing doctors in the United States. Just under half of them are primary care physicians. Even before health reform, the Association of American Medical Colleges estimated that an additional 45,000 primary care physicians would be needed by 2020 to keep up with demand. Already, the availability of primary care physicians varies significantly by region and among states: from 0.9 to 1.0 per 1,000 population in many Southern and Western states to between 1.4 and 2.8 per 1,000 in the Northeast. This means there are about twice as many doctors per 1,000 residents in the Northeast than in states such as Texas. [See the table.]
In response, many medical schools are expanding and four new schools have started enrolling students. Improving the efficiency of medical education could also increase the supply of primary care physicians. Still, it is unlikely there will be enough physicians to replace those who retire over the next 20 years. Moreover, the health reform bill did not include any funds to significantly expand the supply.
Many physicians are concerned that the quality of care patients receive will suffer if patients are treated by less qualified personnel. However, when appropriate, some patients may prefer having the choice to receive treatment for minor conditions in a more convenient setting, such as a retail clinic with evening hours, even if it is by someone other than a traditional medical doctor.
Advanced Practice Nurses. Nurse practitioners and physician assistants have more medical training than registered nurses and are able to deliver some routine medical care without the direct supervision of a physician, including: prescribing or renewing prescriptions for most drugs, ordering blood tests, performing routine medical examinations, monitoring chronic conditions, counseling patients about prevention, and treating colds, sore throats and the flu.
In recent years, many states have expanded the scope of duties that nurse practitioners and physician assistants are allowed to perform. For example, Montana allows nurse practitioners to work without any doctor supervision. By contrast, Texas requires a doctor's direct (on-site) supervision at least 20 percent of the time. Twenty-eight states are debating further loosening restrictions that prevent nurse practitioners and physician assistants from performing more tasks independently.
Three-Year Medical Degrees. A number of medical schools are implementing three-year degree programs as an alternative to the traditional four-year program. It is tempting for a student who has invested significant time and money in medical school to eschew primary care for specialties with far higher earning potential. However, cutting the length of schooling required for primary care practice could reduce a medical student's debt by $35,000 to $50,000. Some critics fear a three-year medical curriculum will compromise students' education, because the fourth year of medical school typically allows students to learn about different specialties.
Three-year programs have already been started at Lake Erie College of Osteopathic Medicine in New York, the University of Calgary and McMaster University in Ontario, Canada. Texas Tech University recently announced it will also offer a three-year option for students willing to commit to primary care:
- Texas Tech's Family Medicine Accelerated Track will recruit 10 to 12 students out of a class of 140.
- Instead of 160 weeks of instruction with breaks, the curriculum will be 151 weeks with limited interruptions.
- Selected students will receive a one-year scholarship, which, along with one less year of instruction, means medical
school could cost half as much as a four-year program.
A forthcoming study from the Carnegie Foundation for the Advancement of Teaching will recommend that all medical schools consider adding three-year degree options. By reducing the amount of time and money necessary to pursue primary care, medical students will be more likely to choose this specialization.
Expanding the Role of Pharmacists. In Europe, Canada and other developed countries, there are three basic classes of drug. In addition to over-the-counter and prescription-only drugs, there are behind-the-counter drugs that pharmacists are allowed to dispense without a prescription. This allows pharmacists to counsel and serve patients who would otherwise frequently make appointments with physicians just to renew prescriptions. The U.S. Food and Drug Administration has considered adding a third class several times since the 1970s but no action has been taken.
Telemedical Practices. Many medical conditions do not require the physical presence of a physician or an actual office visit. Indeed, many conditions could be easily diagnosed, and treatment recommended, over
the telephone. To meet this demand, entrepreneurs are creating nontraditional medical services in which clinical care is available by telephone or through virtual offices staffed by physicians.
Unfortunately, many states have restrictions on telemedicine that make it illegal for a physician in one state to consult with a patient in another state without an initial face-to-face meeting. It is also illegal in most states for a physician who has examined a patient from another state to continue treatment of the patient via the Internet. The physician must be licensed in the state where the patient resides or be guilty of practicing medicine without a license in that state.
Conclusion. The United States is facing a severe shortage of primary care physicians that will only worsen in coming years. Using other medical personnel to free doctors from routine tasks might allow physicians to concentrate on those medical tasks for which they are uniquely qualified.
Devon M. Herrick is a senior fellow with the National Center for Policy Analysis.