Former Congressional Budget Office (CBO) Director Alice Rivlin and Rep. Paul Ryan (R-WI) have offered a proposal to reduce projected Medicare and Medicaid spending. The provisions affecting Medicare are independent of last year's health reform bill, the Patient Protection and Affordable Care Act (ACA). The ACA also cuts Medicare spending significantly in order to fund health insurance for the uninsured.
Evaluating the fiscal impact of either reform requires baseline estimates of Medicare's spending path and of the potential impact of the reform, and an educated guess about the likelihood that the ACA will actually be implemented.
 The Rivlin/Ryan Proposal. This proposal would eventually replace the current Medicare system with a system under which individuals born in 1956 and later would receive a voucher to buy private health insurance. The voucher would be adjusted for age, health risk, geography and recipient income, and would grow at the same rate as per capita gross domestic product (GDP) plus 1 percentage point.
The Rivlin/Ryan Proposal. This proposal would eventually replace the current Medicare system with a system under which individuals born in 1956 and later would receive a voucher to buy private health insurance. The voucher would be adjusted for age, health risk, geography and recipient income, and would grow at the same rate as per capita gross domestic product (GDP) plus 1 percentage point.
Those born in 1955 and earlier, who are 55 and above today, would remain in traditional Medicare and receive a reformed insurance package that combines Medicare Parts A and B, guarantees true catastrophic coverage, includes greater cost sharing and eliminates first dollar Medigap plan coverage. The proposal also would gradually increase the eligibility age for Medicare from 65 years today to 67 by 2032.
The Affordable Care Act. The cost containment measures in the health reform bill passed last year continues the sustainable growth rate (SGR) system that attempts to control payments to physicians under Medicare Part B and makes even more stringent reductions in payments to hospitals and other providers under Part A.
Whereas the Rivlin/Ryan proposal primarily reforms Medicare from the consumers' side of the market, the ACA primarily impacts the supply side. In their 2010 report, the Medicare trustees cautioned that the ACA's reduced payments to providers will be difficult to achieve and may have adverse consequences for patients. The Medicare actuaries noted that Medicare payment rates will fall below Medicaid rates by the end of this decade and could fall further behind other payers in future years. This raises the prospect that some of the elderly and the disabled may have to turn to community health centers and safety-net hospitals for care.
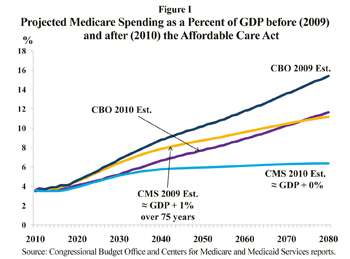
Estimating the Impact of Medicare Spending in Future Years. Figure I presents estimates of Medicare's projected long-run spending – before and after the ACA – by the Congressional Budget Office (CBO) and by the Centers for Medicare and Medicaid Services (CMS) as reported in the Medicare Trustees Reports.
 The top line in Figure I shows the CBO's 2009 projection of Medicare's spending path prior to the ACA, whereas the bottom line shows the CMS projection of Medicare spending after the ACA. Intermediate between these are the 2009 CMS estimate (pre-ACA) and the CBO's 2010 estimate (post-ACA).
The top line in Figure I shows the CBO's 2009 projection of Medicare's spending path prior to the ACA, whereas the bottom line shows the CMS projection of Medicare spending after the ACA. Intermediate between these are the 2009 CMS estimate (pre-ACA) and the CBO's 2010 estimate (post-ACA).
Compared to the 2009 CMS estimate, the 2010 CMS estimate projects Medicare will spend $13.9 trillion, or 24 percent, less over the next 75 years.
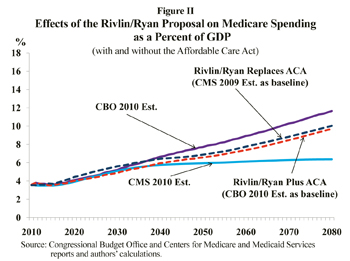
Estimating the Rivlin/Ryan Proposal's Effect on Medicare Spending. Figure II shows estimates derived from the CBO's preliminary scoring of the Rivlin/Ryan proposal, and our alternative estimate. The CBO treats Rivlin/Ryan as an addition to the ACA. The CBO estimates that over the first 10 years, Rivlin/Ryan would reduce Medicare's net federal spending by $110 billion over and above the savings from the ACA. The spending path under Rivlin/Ryan is ultimately greater than the 2010 CMS (post-ACA) estimate because the Rivlin/Ryan voucher grows at GDP + 1 percent, while ACA reimbursements increase at about the same rate as GDP in the long-run.
Figure II also shows our estimate of the effects of the Rivlin/Ryan proposal on Medicare spending assuming that, rather than adding to the ACA, it replaces the ACA reforms. Because we start from a higher baseline (the 2009 CMS estimates), our estimates of Medicare spending based on the Rivlin/Ryan proposal are higher than the CBO estimates that treated Rivlin/Ryan as an ACA add-on.
Long-Run Viability. The ACA essentially imposes price ceilings on Medicare payments to providers. These price controls will lead to fewer health care options and lower quality of care for the Medicare population. In contrast, the Rivlin/Ryan approach would affect both the demand and supply side of the health care market – patients would shop and providers would respond. Provision for low-income beneficiaries in the form of health spending accounts could be structured to keep pace with the new system. The more realistic cost savings resulting from the Rivlin/Ryan proposal could be accomplished without the unintended consequences of price ceilings.
Andrew J. Rettenmaier and Thomas R. Saving are executive associate director and director, respectively, of the Private Enterprise Research Center at Texas A&M University and senior fellows with the National Center for Policy Analysis.